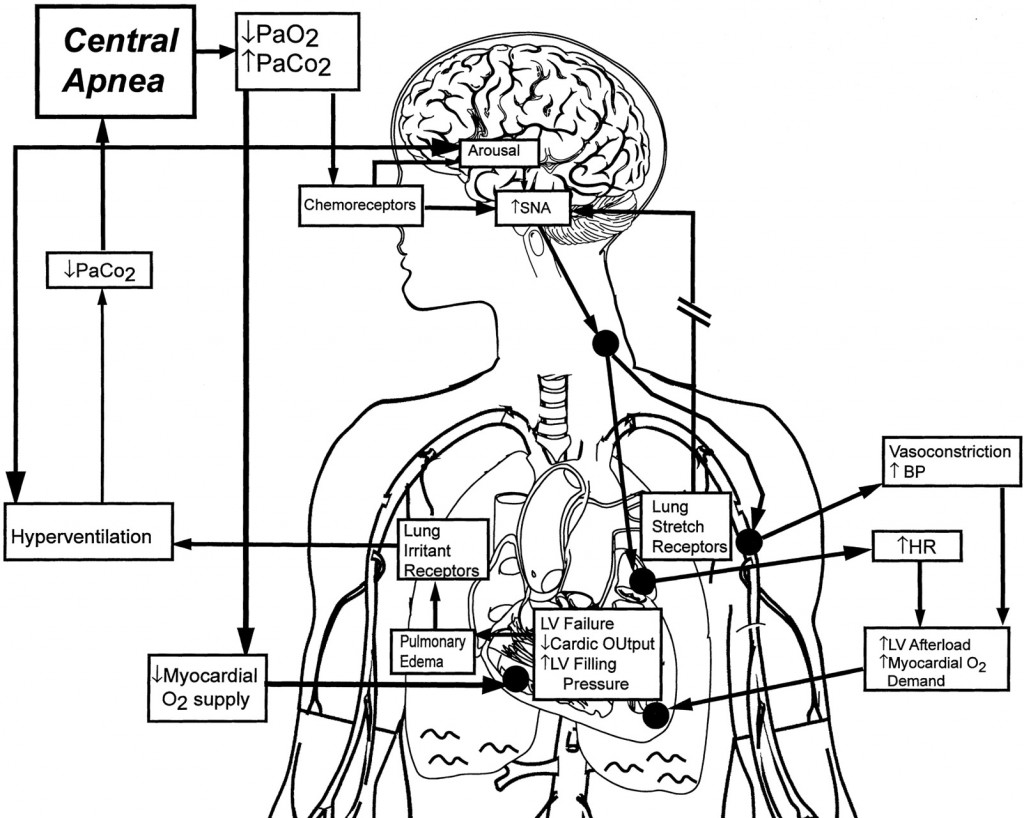
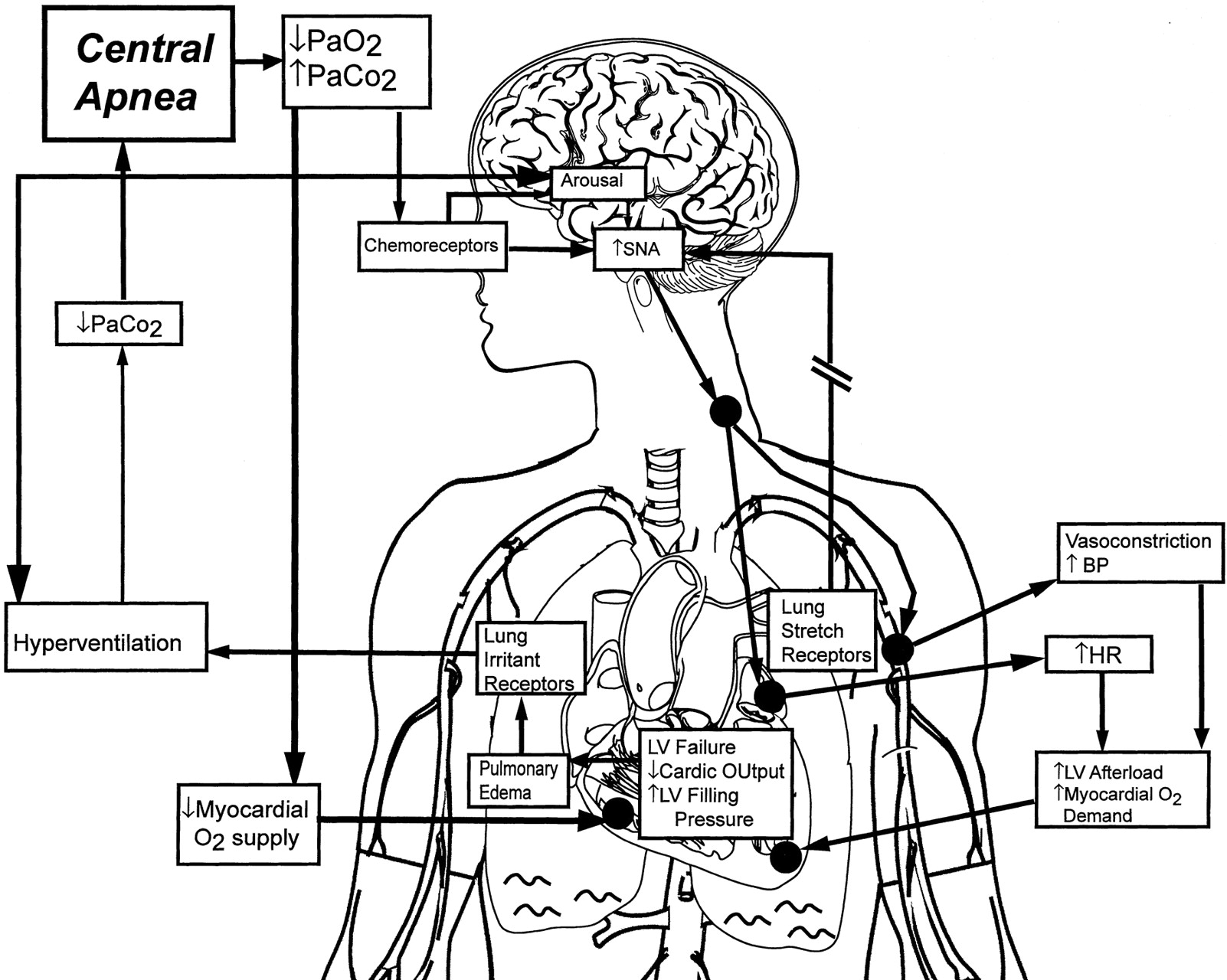
Figure 1. Pathophysiology of central sleep apnea in heart failure (HF). HF leads to increased left ventricular (LV) filling pressure. The resulting pulmonary congestion activates lung vagal irritant receptors, which stimulate hyperventilation and hypocapnia. Superimposed arousals cause further abrupt increases in ventilation and drive PaCO2 below the threshold for ventilation, triggering a central apnea. Central sleep apneas are sustained by recurrent arousals resulting from apnea-induced hypoxia and the increased effort to breathe during the ventilatory phase because of pulmonary congestion and reduced lung compliance. Although central apneas have a different pathophysiology than obstructive apneas and are not associated with the generation of exaggerated negative intrathoracic pressure, they both increase sympathetic nervous system activity (SNA). The consequent increases in blood pressure (BP) and heart rate (HR) increase myocardial O2 demand in the face of reduced supply. This chain of events contributes to a pathophysiological vicious cycle.
Author: admin
Related Articles

admin | No Comment
Mayo Clinic – Central sleep apnea: Definition
Mayo Clinic – Central sleep apnea: Definition, Symptoms, Causes, Risk Factors, Complications Central sleep apnea is a disorder in which
admin | 1 Comment
Sleep Apnea and Heart Disease: Inevitable Consequence Which Can Be Prevented
admin | No Comment
Central Sleep Apnea in Congestive Heart Failure:
admin | No Comment
Central Sleep Apnea Syndromes Treatment & Management
admin | No Comment
Evidence Keeps Mounting on Link Between Apnea and Heart Disease
admin | No Comment
Cheyne-Stokes respiration on ventricular response to atrial fibrillation
admin | No Comment
Adaptive Servo-Ventilation in Patients With Idiopathic Cheyne-Stokes Breathing
admin | No Comment